Placenta holds answers to solving birth injury
Medical errors in the setting of a premature baby can cause brain damage and cerebral palsy
There is a huge misconception that prematurity causes brain damage, and therefore cases of cerebral palsy and developmental delay in the setting of a premature delivery cannot be valid cases of medical malpractice. This is not true. While prematurity is indeed a risk factor for having brain damage, cerebral palsy and/or developmental delay, prematurity alone does not cause these problems. Rather, there is always a physiological cause of brain damage and cerebral palsy (i.e., lack of oxygen, trauma, hemorrhaging, infection, etc.). Sometimes brain damage in the setting of prematurity is unavoidable, and therefore it cannot be attributed to a medical error. However, a significant percentage of the time, even in the setting of a severely premature baby, it is a medical error that brings about a child’s brain damage and associated disabilities. Perhaps the best example of this fact is WVFO’s $229 million-dollar verdict against Johns Hopkins Bayview Medical Center in July of 2019 in the Byrom case. In that birth injury case, the child was born at approximately 26 weeks and 4 days gestation.
Cerebral palsy and PVL - Sheldon's injuries
In 2013, Sheldon Duke was born at 29 weeks and 5 days gestation. For being so premature, Sheldon did fairly well at birth. His Apgar scores were 6 at one minute, and 8 at two minutes. Apgar scores measure how well a baby is doing at birth on a scale of 0 to 10. Thus, Sheldon’s Apgar scores were very reassuring.
One of the big concerns with a baby born at 29 weeks is underdeveloped lungs, which can cause respiratory distress syndrome. Although Sheldon did experience some respiratory distress initially, he did not require the use of ventilator to help him breath. Rather, he was on a simple nasal canula.
A screening head ultrasound was performed on day of life two, which showed no evidence of brain hemorrhaging or edema (i.e., swelling). It appeared from this brain image that Sheldon was neurologically intact at the time.
However, on day of life three, Sheldon’s condition dramatically worsened. He began having labored breathing, which prompted a chest x-ray. The chest x-ray showed atelectasis, which is a sign of pneumonia. Lab work was done and many of the results suggested that Sheldon was suffering from a very significant an infection. As with most premature babies, Sheldon was made “rule out sepsis” upon admission to the NICU, so he was already on some antibiotics. Blood cultures were performed, but they did not show any growth.
The health care providers caring for Sheldon diagnosed him with sepsis, which is an infection of the bloodstream. The sepsis was now causing Sheldon to suffer from severe respiratory distress. As a result of the respiratory distress, Sheldon began experiencing apnea and bradycardia, which is decreased oxygen levels and a low heart rate. On day of life six, another head ultrasound was performed. Unfortunately, the head ultrasound showed massive periventricular leukomalacia or PVL. PVL is when the white matter of the brain is destroyed. Sheldon’s PVL caused him to suffer from spastic quadriplegic cerebral palsy.
Is chorioamnionitis to blame for Sheldon's cerebral palsy?
Sheldon’s parents first reached out to a lawyer in 2015, shortly after Sheldon turned two. Mr. and Mrs. Duke wanted to know why Sheldon ended up so sick when on the first two days of life the doctors were telling them that Sheldon looked great and was headed for a good outcome. Lawyer A agreed to review the case and to try and find some answers for the Dukes.
Lawyer A ordered the medical records for Mrs. Duke’s prenatal care and labor and delivery. He also ordered Sheldon’s newborn records. Importantly, Lawyer A noticed in Mrs. Duke’s records that she had been diagnosed with chorioamnionitis around the time of delivery.
Chorioamnionitis is when the intra-amniotic fluid gets infected. It can cause symptoms in the mother prenatally, and during labor. Those symptoms include, but not are limited to, abdominal pain, foul smelling fluid, fever, maternal tachycardia (i.e., elevated heart rate), fetal tachycardia (i.e., elevated fetal heart rate) and leukocytosis (i.e., an elevated white blood cell count). After delivery, if the chorioamnionitis was severe, there will be evidence of it on placental examination. The placenta will be inflamed, indicating the presence of chorioamnionitis, and the cord can show inflammation too, which is called funisitis.
Lawyer A wondered if Mrs. Duke’s chorioamnionitis was somehow linked to the infection that Sheldon suffered in the newborn period. He had the case evaluated by a few experts. However, those experts did not make any connection between Mrs. Duke’s infection and Sheldon’s infection. Lawyer A promptly rejected the case.
Mrs. Duke felt hopeless.
But, in 2016, she contacted WVFO to solve her son's birth injury case.
The Birth Injury Cold Case team hires a pathologist
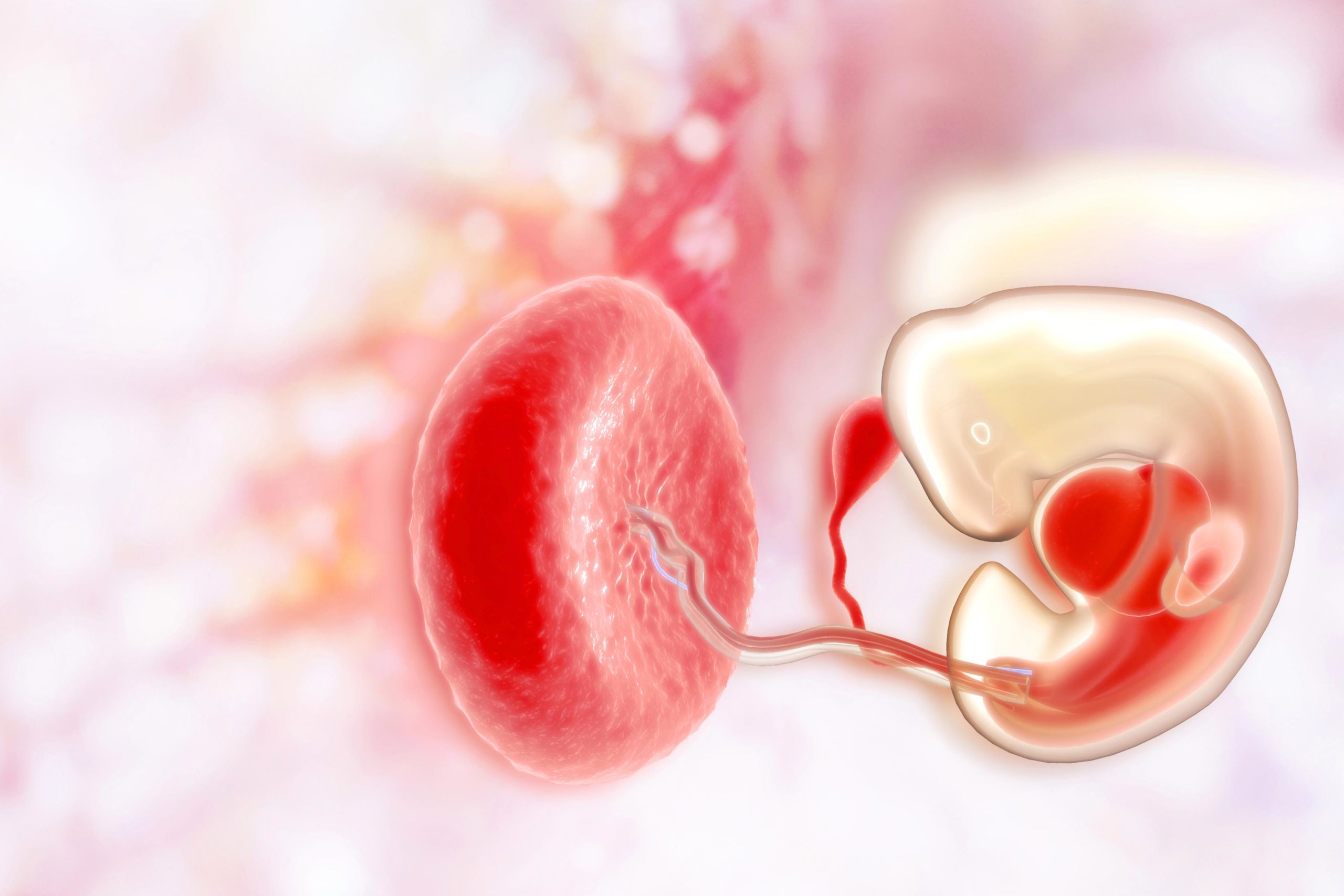
After a baby is born, the placenta is sent to the lab. The pathologist examines the entire placenta, which is called the gross examination. The pathologist also puts portions of the placenta on glass slides and then looks at them under a microscope. This is called the microscopic examination.
Interestingly, the placenta pathology report in Mrs. Duke’s case described “acute chorioamnionitis” and “mild funisitis.” In this setting, the words “acute” and “mild” have very specific meanings. “Acute” essentially means recent. “Mild” means not severe, which also has a connotation of recency. From reading the placental pathology report in Mrs. Duke’s case, the experts who reviewed the case for Lawyer A had a difficult time connecting the dots since it appeared that Mrs. Duke’s chorioamnionitis was timely diagnosed and treated.
But was it?
After performing its own microscopic examination of Mrs. Duke’s and Sheldon’s medical records, WVFO did something Lawyer A did not do. WVFO ordered the placental pathology slides from the Defendant Hospital. Once the slides were received, they were promptly sent to a preeminent placental pathologist who had authored several peer-reviewed articles on the topic of chorioamnionitis.
Necrotizing vaculitis
The pathology expert retained by WVFO made a stunning discovery. According to his review of the placental pathology slides, there was evidence of a long-standing placental infection that had led to part of the placenta being eaten away by the bacteria. This was at odds with the placental pathology report in the records and suggested that there had been a chronic infection of Mrs. Duke’s placenta. WVFO immediately went back to the records to see if an opportunity to catch this chronic infection was missed by the Defendant Hospital. Did this error cause Sheldon's birth injury?
The Birth Injury Cold Case lawyers connect the dots
Three days before being admitted in pre-term labor secondary to her chorioamnionitis, Mrs. Duke had presented to the Defendant Hospital with severe abdominal pain. Because the Defendant health care providers believed Mrs. Duke had a urinary tract infection blood was drawn from Mrs. Duke and sent to the lab. That blood work showed that Mrs. Duke had an elevated white blood cell count. Furthermore, the electronic fetal heart rate monitoring exhibited fetal tachycardia. As such, Mrs. Duke had three of the key symptoms of chorioamnionitis. However, the Defendant health care providers erroneously diagnosed Mrs. Duke with a urinary tract infection, gave her antibiotics that do not treat chorioamnionitis, gave her pain medication to mask her abdominal pain, and discharged her home.
Over the next three days, Sheldon sat in a hostile and infected intrauterine environment, where he contracted the infection that would later make him so unstable to the point of suffering PVL and brain damage.
WVFO had the case reviewed by experts in obstetrics and gynecology, maternal-fetal medicine, and neonatology. All of the experts were unanimous that the Defendant Hospital and the Defendant health care providers had breached the standard of care by not diagnosing and treating Mrs. Duke’s chorioamnionitis on the admission three days before her delivery admission. The experts also all agreed that had the chorioamnionitis been timely diagnosed and treated three days earlier that Sheldon would not have been infection, would not have crashed on day of life three, would not have suffered PVL, and would not have suffered brain damage and cerebral palsy.
A birth injury lawsuit was filed in 2017 and ultimately settled for millions of dollars.
CASE CLOSED.
